AI in Resource Allocation for Supply Chain Recovery
Post Summary
AI enhances supply chain recovery by optimizing resource allocation, automating processes, and enabling real-time risk detection and decision-making.
AI uses machine learning and data analytics to dynamically balance inventory, optimize routes, and allocate resources efficiently during disruptions.
Benefits include faster recovery times, improved resilience, reduced downtime, and enhanced operational efficiency.
Challenges include high implementation costs, data privacy concerns, and the need for skilled personnel to manage AI systems.
Technologies include machine learning, big data analytics, digital twins, and intelligent decision support systems.
Organizations can prepare by forming cross-functional AI committees, investing in AI tools, and ensuring robust cybersecurity and compliance measures.
AI is transforming how healthcare systems recover from supply chain disruptions, such as natural disasters, cyberattacks, or public health crises. By analyzing data like purchasing trends, patient needs, and external risks, AI can predict shortages, optimize inventory, and suggest alternative suppliers or products. This reduces waste, speeds up recovery, and ensures critical supplies like medications and ventilators reach where they're needed most. AI also strengthens cybersecurity by flagging high-risk vendors and safeguarding patient data during crises.
Key takeaways:
- Forecasting demand: AI predicts supply needs with 85% accuracy, compared to 65% with traditional methods.
- Inventory management: Automates reordering, prevents waste, and ensures 99% product availability.
- Cybersecurity integration: Identifies supplier risks and aligns recovery efforts with compliance standards.
- Human oversight: Committees review AI outputs to ensure patient safety and ethical decision-making.
AI-driven tools like Censinet RiskOps™ have already helped healthcare systems cut costs, reduce errors, and improve efficiency during supply chain recovery efforts.
How AI Supports Healthcare Supply Chain Recovery
Forecasting Demand and Capacity During Disruptions
AI plays a crucial role in predicting short-term needs for supplies, hospital beds, and staff by analyzing a mix of historical data, electronic health records, seasonal illness patterns, and external indicators like weather forecasts or outbreak data. For instance, AI models trained on previous flu seasons can detect a spike in respiratory cases early and recommend stocking up on ventilator circuits, antivirals, and ICU beds in specific areas - weeks before shortages arise. These systems continuously refine their forecasts by incorporating new data [2]. During recovery phases, AI can estimate patient arrivals, expected length of stay, and care intensity, helping health systems allocate travel nurses, float pools, or step-down beds more effectively to prevent bottlenecks. U.S. healthcare providers can integrate these AI tools with electronic health records and labor scheduling platforms, enabling daily surge planning and preemptive patient transfers. These insights allow for real-time inventory adjustments and smarter substitution strategies.
Managing Inventory and Finding Substitute Products
With accurate demand forecasts, AI can monitor inventory levels, usage patterns, lead times, and expiration dates to recommend when and how much to reorder. It can also identify opportunities for cross-facility transfers, reducing waste and avoiding stockouts. For example, if one hospital has excess oncology drugs or N95 masks nearing expiration, AI can suggest redistributing these to another facility experiencing higher demand instead of placing new orders. This approach has reportedly cut medical supply waste by 30–40% while maintaining a 99% availability rate for critical products [2]. When primary items are unavailable, AI can analyze clinical guidelines, product attributes, and value-analysis data to propose alternative options that meet safety and performance standards. However, it’s essential for clinicians and review committees to evaluate these suggestions, define constraints - such as avoiding substitutions for high-risk implants - and establish clear rules to ensure patient safety and regulatory compliance during shortages.
Evaluating Supplier and Cyber Risk
AI also helps healthcare systems assess supplier reliability by analyzing factors like delivery performance, quality records, fill rates, financial health, geopolitical risks, and production capacity. This information generates dynamic risk and resilience scores, enabling supply chain leaders to identify vendors best equipped to handle surges and flag those requiring contingency plans or diversification. AI can simulate potential disruptions - such as factory shutdowns or cyberattacks - and predict their impact on product availability and costs. This analysis helps prioritize strategies like activating alternative suppliers, sourcing substitute products, or building inventory buffers. Additionally, AI enhances cybersecurity within the supply chain by reviewing vendor security questionnaires, tracking past incidents, monitoring vulnerability feeds, and analyzing network behavior to identify high-risk third parties. Tools like Censinet RiskOps™ embed these risk scores and mitigation strategies directly into supply workflows, aligning supply chain recovery efforts with cybersecurity and compliance goals.
Building an AI-Driven Recovery Framework
Setting Recovery Goals and Constraints
Before deploying AI, healthcare organizations need to translate their business continuity plans into clear, measurable recovery targets. This involves setting precise benchmarks, such as the maximum acceptable downtime for critical supplies, target fill rates (e.g., ensuring 99% availability for high-risk items), and acceptable backorder thresholds. Across the U.S., leading health systems conduct workshops with key stakeholders - supply chain leaders, pharmacy directors, clinical staff, risk managers, IT security teams, and finance professionals - to prioritize objectives. The top priorities are typically patient safety and service continuity, followed by cost management and operational efficiency.
These goals must also account for specific constraints. For example, clinical safety rules could include "do-not-substitute" lists for certain implants or medications. Regulatory guidelines might encompass FDA device standards, Joint Commission accreditation requirements, and HIPAA compliance. Cybersecurity constraints could involve minimum vendor risk scores or prohibitions against sourcing from suppliers with unresolved security issues. Other practical limits include budget caps in U.S. dollars, storage capacity in square feet, and cold-chain requirements in cubic feet. Encoding these parameters into AI optimization tools ensures that recovery decisions align with patient safety, compliance, and operational boundaries. Once goals and constraints are clearly defined, the next step is to integrate AI with critical data sources to bring these plans to life.
Connecting AI to Critical Data Sources
AI systems thrive on detailed, real-time data drawn from across the organization. Key sources include electronic health records (EHR), enterprise resource planning (ERP) systems, procurement platforms, and logistics tools. These systems provide essential data such as utilization patterns, patient census numbers, surgical schedules, inventory levels, lead times, fill rates, and shipment statuses.
Cybersecurity and third-party risk management platforms add another layer of critical information. Vendor security ratings, incident histories, and device or application risk profiles help AI systems steer clear of high-risk suppliers during recovery efforts. Platforms like Censinet RiskOps™ can continuously feed standardized risk indicators into AI-driven sourcing and allocation tools, ensuring that rapid substitutions or new vendor onboarding maintain compliance with established risk controls. Healthcare organizations typically implement read-only integrations via HL7/FHIR APIs and standard ERP connectors in HIPAA-compliant environments.
"Healthcare is the most complex industry... You can't just take a tool and apply it to healthcare if it wasn't built specifically for healthcare." – Matt Christensen, Sr. Director GRC, Intermountain Health [1]
To minimize disruptions to clinical workflows, AI outputs - such as forecasts, risk scores, recommended order quantities, or substitution options - are embedded directly into existing ERP or EHR interfaces as decision-support widgets. This approach avoids forcing clinicians or buyers to navigate new standalone tools. When cyber and third-party risk systems are integrated into sourcing workflows, AI can automatically flag or deprioritize high-risk vendors, sparing staff the need to manually check separate dashboards.
Establishing Governance and Human Oversight
With integrated data streams and well-defined constraints in place, strong human oversight ensures that AI recommendations align with clinical and cybersecurity standards. Effective AI programs establish a cross-functional AI Supply Chain Recovery Steering Committee that includes representatives from supply chain, pharmacy, nursing leadership, IT, information security, privacy, compliance, and finance. This committee is responsible for approving AI use cases, setting acceptable risk thresholds, defining performance indicators, and monitoring for unintended consequences. On a day-to-day basis, supply chain leaders manage AI-driven allocation and inventory tools, while the Chief Information Security Officer (CISO) and risk teams oversee cybersecurity and vendor risk management - often using platforms like Censinet for continuous monitoring. Clinical leaders validate substitution rules and protocols to ensure they meet patient safety standards.
Human-in-the-loop checkpoints are embedded at critical decision points. For instance, if AI suggests reallocating ventilators or N95 masks across facilities, clinical and operational leaders must review and approve the decision before implementation. Escalation rules are clearly defined: any decision that could affect the standard of care or involve off-formulary substitutions requires review by a clinician or pharmacy lead. To build trust, AI recommendations are accompanied by transparent explanations, such as predicted patient census, historical usage rates, and supplier risk scores. This transparency allows staff to challenge or override AI outputs when necessary. Training programs help clinicians and supply chain staff understand AI's strengths and limitations, while incident-reporting mechanisms enable them to flag questionable outputs for review and adjustment. Ethical guidelines, aligned with U.S. bioethics and anti-discrimination standards, ensure AI prioritizes scarce resources fairly, avoiding decisions based on non-clinical factors like insurance status or demographics.
An internal model risk management function or committee oversees algorithm updates, validation processes, and incident reviews. This ensures accountability and traceability for AI-driven decisions, following governance practices similar to those used in financial modeling. This structure keeps patient safety and equity at the forefront while allowing human teams to focus on strategic oversight and solving complex challenges.
sbb-itb-535baee
Measuring AI's Effect on Recovery Operations
Tracking Recovery Performance Metrics
To evaluate how AI impacts recovery in supply chain operations, it's essential to track specific metrics like time to recovery (TTR), fill rate, stockout frequency, inventory efficiency, decision adoption rate, and cost to serve.
Time to recovery (TTR) refers to the time it takes to restore service levels after a disruption, such as a critical backorder or a cyber incident. This can be measured in hours or days and compared against pre-AI baselines over a 6–12 month period to gauge improvement.
Metrics like fill rate and product availability help determine if AI ensures the steady flow of critical supplies during crises. For example, AI-enabled medical supply chains have achieved 99% product availability by integrating predictive forecasting with inventory optimization [2]. Other key indicators include the number and duration of critical stockouts (measured monthly or per 1,000 patient days), inventory efficiency (e.g., days on hand, turnover rates, and waste levels), and the AI-supported decision rate, which tracks how often AI recommendations are applied to purchasing, substitutions, or allocation decisions.
Another critical metric is the cost to serve during disruptions, which includes expenses like premium freight, emergency purchases, and overtime. Monitoring these costs highlights how AI can help reduce operational expenses [3][4].
To get the most out of these metrics, segment data by facility, service line, and product priority. Dashboards can then display trends before and after AI implementation. For a more controlled analysis, consider testing AI in a limited scope - such as specific hospitals or product categories - and comparing results to non-AI environments. Alternatively, tabletop simulations can provide insights into how AI affects response times and shortage prevention compared to traditional methods. These metrics collectively help assess AI's role in protecting patient safety and maintaining compliance during recovery efforts.
Monitoring Patient Safety and Compliance
AI-driven systems play a critical role in patient safety by preventing supply chain issues from disrupting care. Metrics like procedure delays, substitution-related adverse events, and safety-critical stockouts are key indicators. For example, track how often procedures are delayed or canceled due to supply shortages (per 1,000 procedures) and monitor adverse events tied to medication or device substitutions. Additionally, keep an eye on infection or complication rates when sterile supplies run short. During the COVID-19 pandemic, AI-powered logistics helped avoid stockouts of essential items like PPE and ventilators, ensuring uninterrupted care [2].
On the compliance and cybersecurity side, monitor cyber incidents that affect supply chain systems or AI tools. Evaluate how quickly AI systems flag recalls, identify affected lots, and suggest safe substitutes. Maintain detailed audit trails for AI-assisted decisions, ensuring proper documentation and human approval when necessary. Tools like Censinet RiskOps™ can help centralize risk assessments, cybersecurity benchmarks, and vendor monitoring. These platforms are especially useful for managing risks tied to protected health information (PHI), clinical applications, and device data. By integrating AI-related risks into broader enterprise risk strategies, healthcare organizations can maintain a proactive approach to recovery operations [4].
Improving AI Models Through Feedback
After significant disruptions, it's essential to review AI performance by comparing recommendations to actual outcomes. Identify gaps, document override reasons, and feed this data back into the system to refine model accuracy. For example, public healthcare supply chains using AI have reported lower stockout rates and reduced excess inventory, though results vary depending on implementation [5].
Feedback from staff - whether supply chain managers, clinicians, or risk specialists - is invaluable. Metrics like the override rate, which measures how often staff reject AI suggestions, can reveal areas for improvement. Reasons for overrides, such as clinical judgment, data quality issues, or ethical concerns, should be documented to guide refinements. Tracking trends in key metrics like stockouts, emergency spending, and data errors over time can also signal whether AI systems are improving. One provider reported a 30% reduction in data errors after adopting AI-based integration systems [3].
Adding AI to Healthcare Risk and Supply Chain Programs
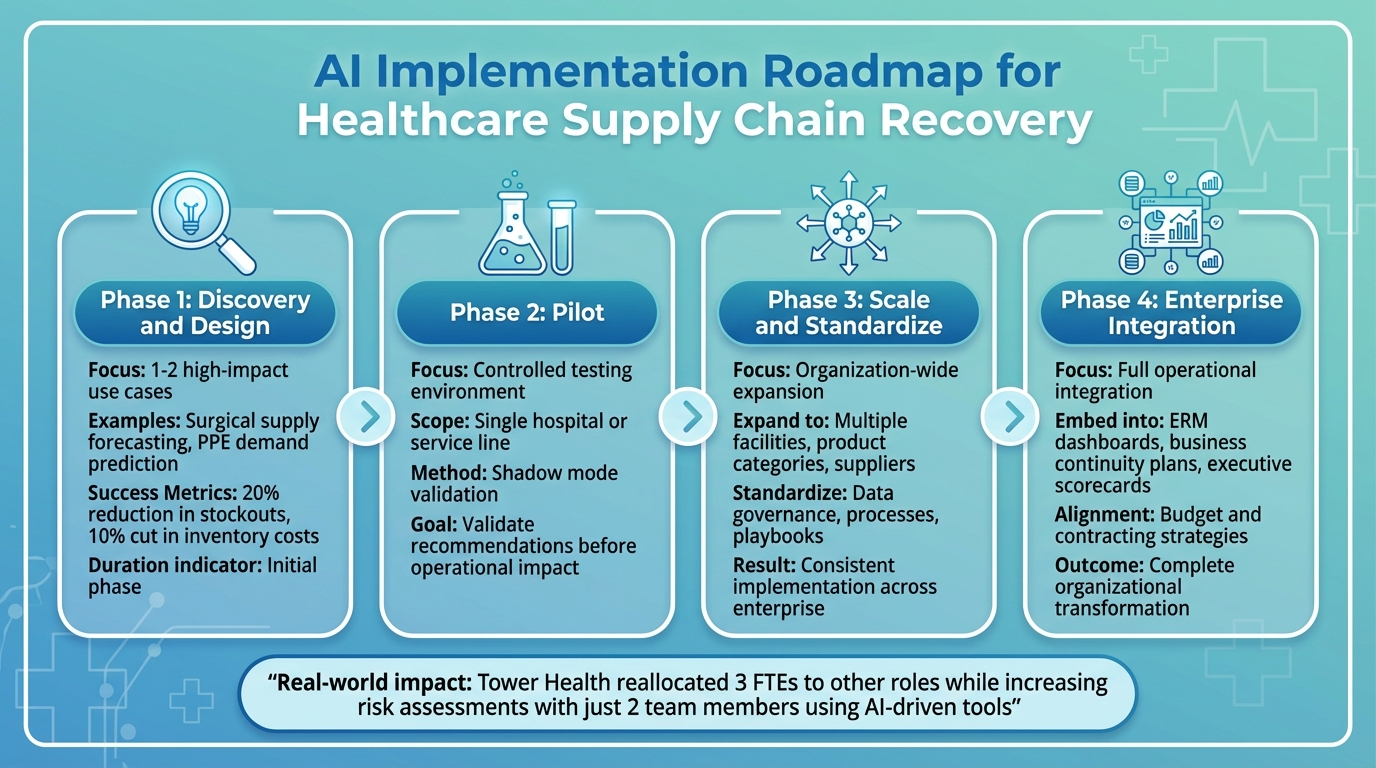
4-Phase AI Implementation Framework for Healthcare Supply Chain Recovery
Connecting AI to Enterprise Risk Management
When integrating AI into healthcare systems, tying it closely to your Enterprise Risk Management (ERM) framework is a smart move. Start by pinpointing specific AI applications - like demand forecasting, inventory management, or supplier risk scoring - and match each to a risk category in your ERM register (e.g., clinical, supply chain, cybersecurity/PHI, financial, or regulatory). Assign clear ownership of these risks and define measurable thresholds, such as acceptable forecast errors or stockout probabilities.
Incorporate AI-powered early-warning signals into your continuity plans to activate pre-designed playbooks for situations like drug shortages, PPE demand spikes, or vendor cybersecurity breaches. To ensure these systems work as intended during actual disruptions, test them in tabletop exercises that involve both clinical and supply chain leaders.
Platforms like Censinet RiskOps™ can play a crucial role by embedding cyber-risk assessments into your ERM framework. This ensures that AI vendors and data-sharing partners meet strict security standards to protect patient data and PHI. By linking recovery operations with broader risk strategies, this approach lays the groundwork for a phased and secure AI rollout.
Planning Your AI Implementation
A phased approach to AI implementation not only reduces risks but also builds confidence across the organization.
- Phase 1 (Discovery and Design): Begin with one or two straightforward, high-impact use cases, such as using AI to forecast demand for surgical supplies or PPE. Define clear success metrics, like reducing stockouts by 20% or cutting inventory costs by 10% [2].
- Phase 2 (Pilot): Test AI in a controlled environment, such as a single hospital or service line. Start in "shadow mode" to validate the system’s recommendations without immediate operational impact.
- Phase 3 (Scale and Standardize): Once the pilot achieves its goals, expand the AI model to other facilities, product categories, and suppliers. Standardize data governance, processes, and playbooks across the organization.
- Phase 4 (Enterprise Integration): Fully embed AI outputs into ERM dashboards, business continuity plans, and executive scorecards. This ensures AI-driven decisions align with broader budgeting and contracting strategies.
For example, Tower Health implemented Censinet RiskOps™ and restructured its workforce, reallocating three full-time employees to other roles while increasing the number of risk assessments with just two team members. This shift highlights the efficiency gains possible with AI [1]. As you scale, focus on addressing AI-related risks and fostering trust among stakeholders.
Managing AI Risks and Building Stakeholder Trust
To manage risks effectively and build trust, establish an AI governance committee with members from supply chain, clinical, IT, cybersecurity, compliance, finance, and risk management. This group should approve use cases, review AI models, and oversee monitoring and incident response. Require AI vendors to undergo thorough third-party risk assessments for security, privacy, reliability, and resilience. Tools like Censinet can simplify this process by streamlining due diligence, contract evaluations, and ongoing monitoring.
Document and stress-test AI models to validate their performance, and set clear criteria for human intervention when needed. Ensure datasets represent diverse patient populations and care sites to avoid biases that could negatively impact smaller or rural facilities during recovery efforts.
Transparent communication is key. Explain to clinicians and operational staff how the AI system works, how it generates recommendations, and where human oversight fits in. This not only reduces skepticism but also ensures smooth integration. Strong governance enhances both operational resilience and the quality of care.
For instance, Baptist Health replaced spreadsheets with an AI-driven risk management system, gaining access to a broader hospital network for collaborative risk mitigation. Similarly, Faith Regional Health leverages cybersecurity benchmarking to advocate for resources and demonstrate compliance with industry best practices [1].
FAQs
How does AI enhance the healthcare supply chain during crises?
AI plays a crucial role in strengthening the healthcare supply chain during emergencies by refining risk management, improving resource distribution, and supporting real-time decision-making. These tools enable organizations to pinpoint weaknesses, respond effectively to disruptions, and maintain smooth operations in critical areas.
Take Censinet RiskOps™ as an example. This AI-driven platform helps healthcare providers simplify risk assessments, tackle supply chain issues ahead of time, and protect vital resources. As a result, it ensures that patient care continues uninterrupted, even under the toughest conditions.
Why is human oversight important in AI-driven healthcare supply chain management?
Human involvement plays a key role in managing AI-driven healthcare supply chains, ensuring decisions are not only precise but also ethical and context-sensitive. While AI is great at crunching numbers and spotting patterns, it’s the human touch that validates these outputs, handles the gray areas, and makes informed choices in complex or delicate situations.
This partnership between humans and AI reduces risks, tackles real-world challenges, and keeps the technology aligned with both organizational goals and patient care needs. By blending AI’s speed and analytical power with human judgment, supply chain operations can achieve a balance of efficiency and dependability.
How does AI improve cybersecurity in healthcare supply chains?
AI is transforming cybersecurity in healthcare supply chains by automating the detection of vulnerabilities, keeping a constant eye on risks, and evaluating threats from both third-party vendors and internal operations. These advancements allow healthcare organizations to tackle potential issues head-on, lighten the load of manual tasks, and bolster their overall security defenses.
With AI, organizations can assess their cybersecurity readiness, simplify risk management workflows, and safeguard critical assets such as patient data and medical device systems. This forward-thinking strategy helps maintain resilience and reduces interruptions in essential supply chain activities.
Related Blog Posts
Key Points:
What is the role of AI in supply chain recovery?
Role of AI: AI plays a critical role in supply chain recovery by optimizing resource allocation, automating repetitive tasks, and enabling real-time risk detection. It enhances decision-making during disruptions and ensures faster recovery by leveraging data-driven insights.
How does AI improve resource allocation in supply chains?
Resource Allocation: AI uses machine learning and advanced algorithms to dynamically balance inventory, optimize logistics routes, and allocate resources efficiently. This ensures that supply chains remain agile and responsive during crises.
What are the benefits of AI-driven supply chain recovery?
Benefits:
- Faster recovery times, reducing downtime from days to hours.
- Improved resilience and adaptability in rapidly changing environments.
- Enhanced operational efficiency through automation and intelligent decision-making.
- Reduced waste and improved sustainability by optimizing resource use.
What challenges exist in implementing AI for supply chain recovery?
Challenges:
- High implementation costs and the need for significant upfront investment.
- Data privacy and security concerns, especially when handling sensitive information.
- Lack of skilled personnel to manage and maintain AI-driven systems.
- Resistance to change within organizations and legacy system integration issues.
What technologies support AI in supply chain recovery?
Technologies:
- Machine Learning: Enables predictive analytics and dynamic resource allocation.
- Big Data Analytics: Processes vast amounts of data to generate actionable insights.
- Digital Twins: Simulates supply chain scenarios to optimize resilience and efficiency.
- Intelligent Decision Support Systems: Facilitates real-time decision-making during disruptions.
How can organizations prepare for AI-driven supply chain recovery?
Preparation Steps:
- Establish cross-functional AI committees to oversee implementation and risk management.
- Invest in AI-driven tools for inventory management, logistics, and resource allocation.
- Ensure robust cybersecurity measures to protect data and systems.
- Train staff on AI technologies and foster a culture of innovation and adaptability.


